(BMJ) - An 18-day-old baby with normal birth hx presented with a new rash of sharply demarcated, red, irregularly-shaped papules and plaques. The baby appeared well w/o lymphadenopathy or organomegaly. Blood work confirmed the diagnosis. What is it?

|
Tinea corporis
|
|
Neonatal psoriasis
|
|
Staphylococcal scalded skin syndrome
|
|
Herpesvirus 6-associated urticaria multiforme
|
|
Allergic reaction to diaper cream
|
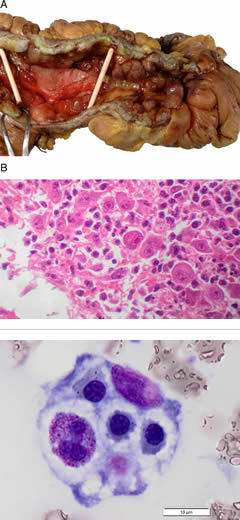
(BMJ) - A 21-yo man on azathioprine for Crohn dz presents w/ fever + pancytopenia. No response to abx, GCSF, or AZA withdrawal. Labs: high TGs, ferritin; low fibrinogen. Bone marrow: unusual macrophage. Ileum histology: CMV infection. What is the diagnosis?
|
Multiple myeloma
|
|
Arsenic poisoning
|
|
Hemophagocytic lymphohistiocytosis
|
|
Azathioprine toxicity
|
|
Hepatitis C
|
(BMJ) - A 64-yo woman presented w/ weakness, UTI, and vesicular eruption on left lower back and right thigh. PMHx: type 2 DM, prior stroke, and polymyositis. Medication: prednisone 20 mg daily. Labs: CRP was 3.7, others were WNL. What is the rash?

|
Behçet disease
|
|
Herpes zoster duplex bilateralis
|
|
Drug reaction
|
|
Contact dermatitis
|
|
Herpes simplex
|
(BMJ) - A 30-yo cyclist skidded on a wet road and struck his head on a curb. He was alert and oriented with normal vital signs. Blood was noted originating from the left external auditory meatus, leaving a halo on the sheet. What is the diagnosis?

|
Basilar skull fracture
|
|
Maxillary sinus fluid leak
|
|
Hemorrhagic mastoiditis
|
|
Ear foreign body
|
|
Ruptured tympanic membrane
|
(BMJ) - A 2.7-kg boy was delivered as breech vaginal birth after uncomplicated pregnancy. The infant was well w/ normal exam except for multiple white nodules along alveolar ridge of maxilla that did not interfere with nursing. What are they?

|
Primordial cysts
|
|
Mucoceles
|
|
Bohn nodules
|
|
Natal teeth
|
|
Epstein pearls
|
A 79-yo woman with PMHx of Wegener’s granulomatosis presented with hyperpigmentation of arms, face, and legs. Medication: methotrexate. Adrenal function and ACTH level normal. What is the diagnosis?

|
Methotrexate-associated hyperpigmentation
|
|
Cushing disease
|
|
Addison disease
|
|
Acanthosis nigricans
|
|
Solar lentigo
|
