(BMJ) - A 73-yo man presented w/ toe ulceration x 3 mo that did not respond to antifungal tx. In the past mo, he also noted a 7-kg weight loss. Exam: Enlarged, red, nontender mass at tip of right 5th toe. What is the diagnosis?

|
Granuloma annulare
|
|
Glomus tumor
|
|
Syphilis
|
|
Onychocryptosis with paronychia
|
|
Rhabdomyosarcoma
|
(BMJ) – A 4-yo boy presented w/ a hx of isolated left-facial flushing during meals since the age of weaning. Sx were triggered by sweet foods (fruit, candy). Skin prick tests: negative. Birth hx: failure to progress requiring forceps delivery. What is the diagnosis?

|
Food allergy
|
|
Niacin exposure
|
|
Erythema infectiosum
|
|
Frey syndrome
|
|
Rosacea
|
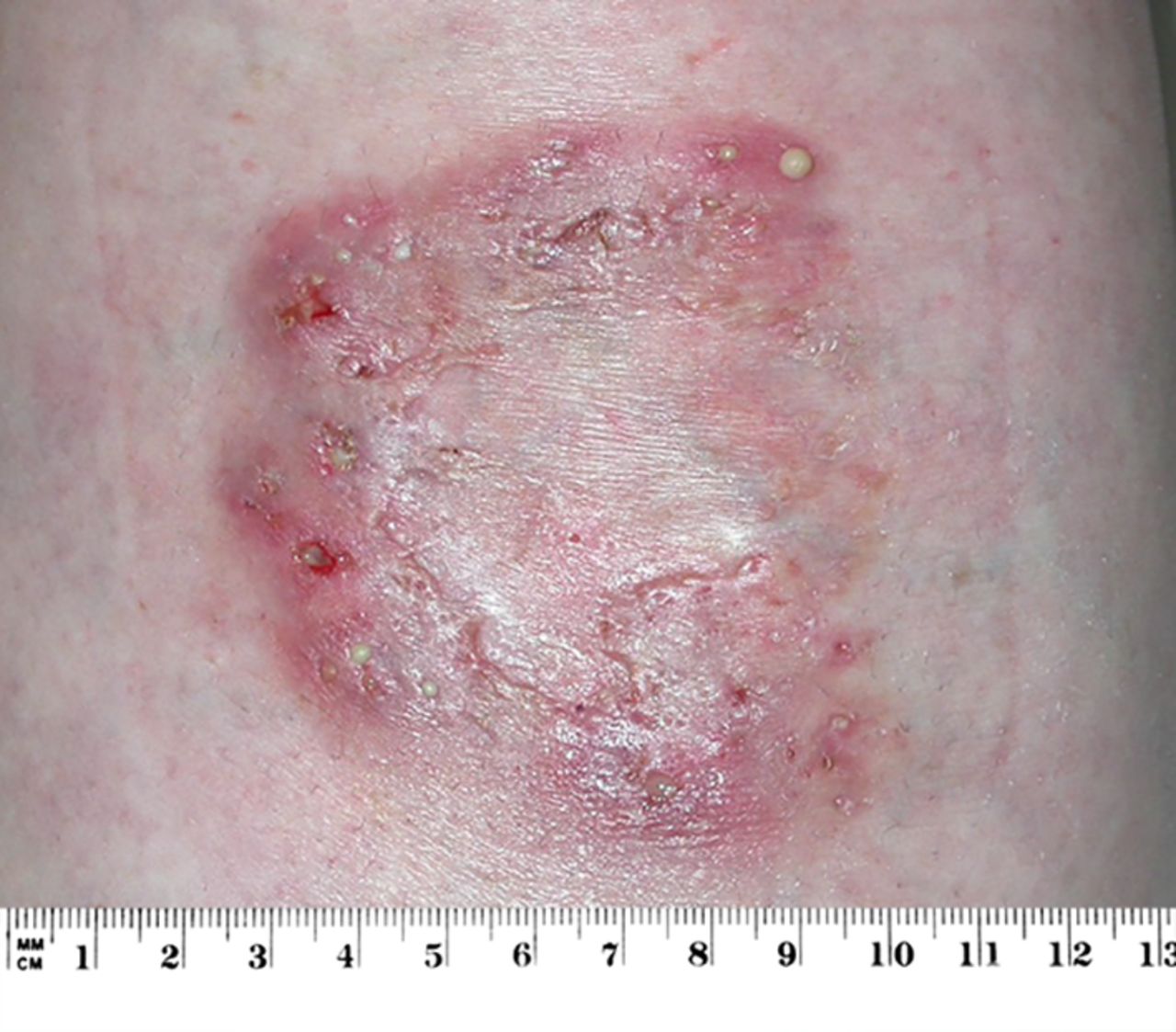
(BMJ) – A 41-yo female w/ poorly controlled Crohn disease presented w/ a painful lesion on her left shin that started as a small red blemish 8 wks prior. Exam: ulcer w/ purulent base & violaceous border. What is the diagnosis?
|
Squamous cell carcinoma
|
|
Ecthyma
|
|
Pyoderma gangrenosum
|
|
Vasculitis
|
|
Venous stasis ulcer
|
(BMJ) – A healthy 45-yo male presented w/ a 1-wk history of unilateral headache, which he described as “the worst ever,” associated w/ nausea & photophobia. Exam: marked epiphora & corneal edema of right eye. Visual acuity: hand movements. Pupil: fixed/mid-dilated. What is the diagnosis?

|
Acute primary angle-closure glaucoma
|
|
Ocular migraine
|
|
Subarachnoid hemorrhage
|
|
Meningitis
|
|
Cluster headache
|
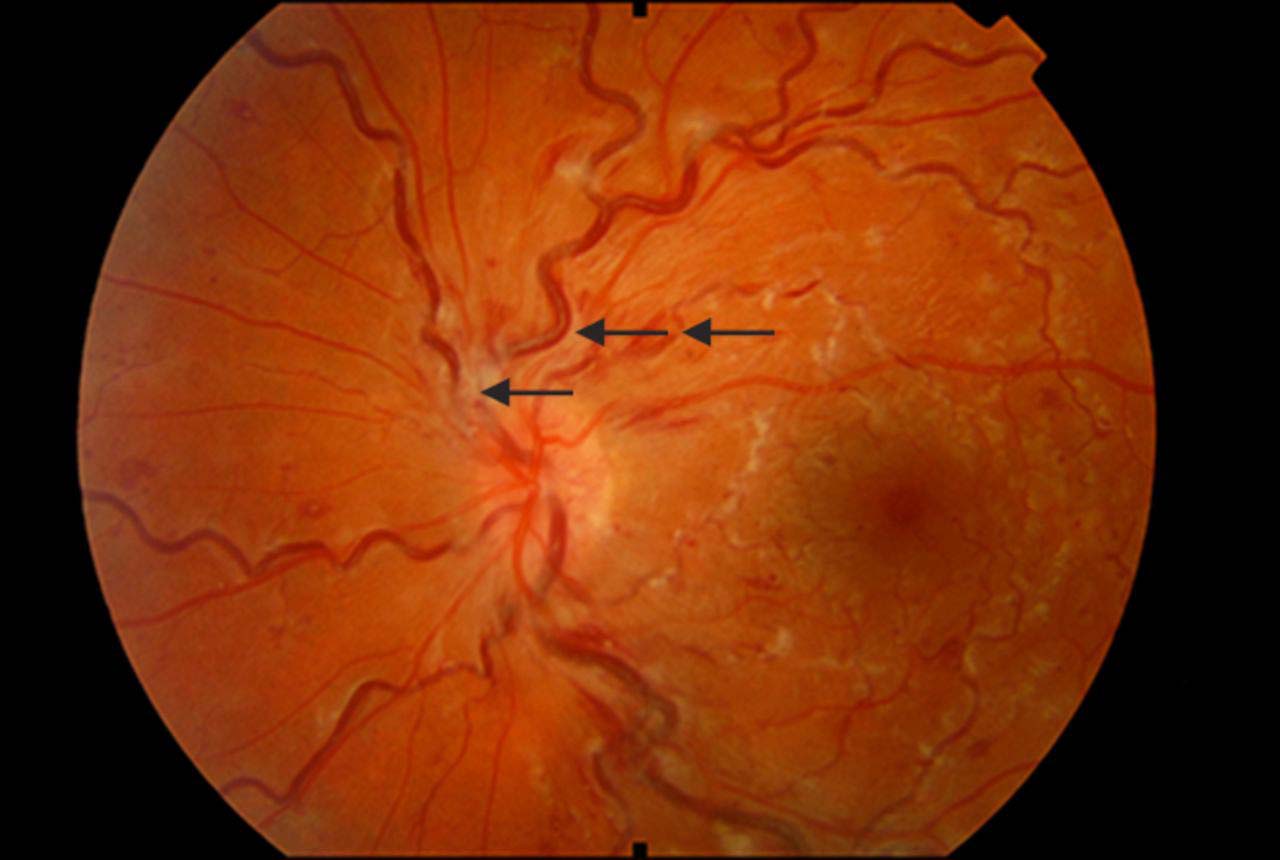
(BMJ) - An 18-yo healthy female on desogestrel contraceptive pills presented w/ sudden onset of blurred vision in her left eye. Fundoscopy revealed tortuous veins, exudates, and hemorrhages. What is the diagnosis?
|
Ocular migraine
|
|
Behcet vasculitis
|
|
Toxoplasmosis
|
|
Branch retinal artery occlusion
|
|
Central retinal vein occlusion
|
(BMJ) - A woman w/ well-controlled epilepsy presented w/ recurrent blistering, crusty lesions that were associated w/ high fevers that triggered seizures. She responded to repeated courses of antistaphylococcal abx, but each time the lesions recurred w/in 1 wk of stopping tx. What is it?
|
Panton-Valentine leucocidin-positive S aureus
|
|
Fixed drug reaction
|
|
Pemphigus vulgaris
|
|
Herpes simplex
|
|
Sweet syndrome (acute febrile neutrophilic dermatosis)
|
(BMJ) - A 32-yo woman presented w/ temporomandibular joint dysfunction. She demonstrated Gorlin sign (the ability to touch the nose w/ the tip of the tongue). What underlying disease was suspected?

|
Cutis laxa
|
|
Marfan syndrome
|
|
Fibromyalgia
|
|
Ehlers-Danlos syndrome
|
|
Pseudoxanthoma elasticum
|
(BMJ) – A child presented to the emergency department w/ circular burns to both hands. Exam revealed 2 partial-thickness burns (0.5%-1% of total body surface area). PMH: none. Meds: none. What caused the burns?

|
Stevens-Johnson syndrome
|
|
Pemphigus vulgaris
|
|
Aerosol spray exposure (“frosting”)
|
|
Staphylococcal scalded skin syndrome
|
|
Cold exposure (frostbite)
|
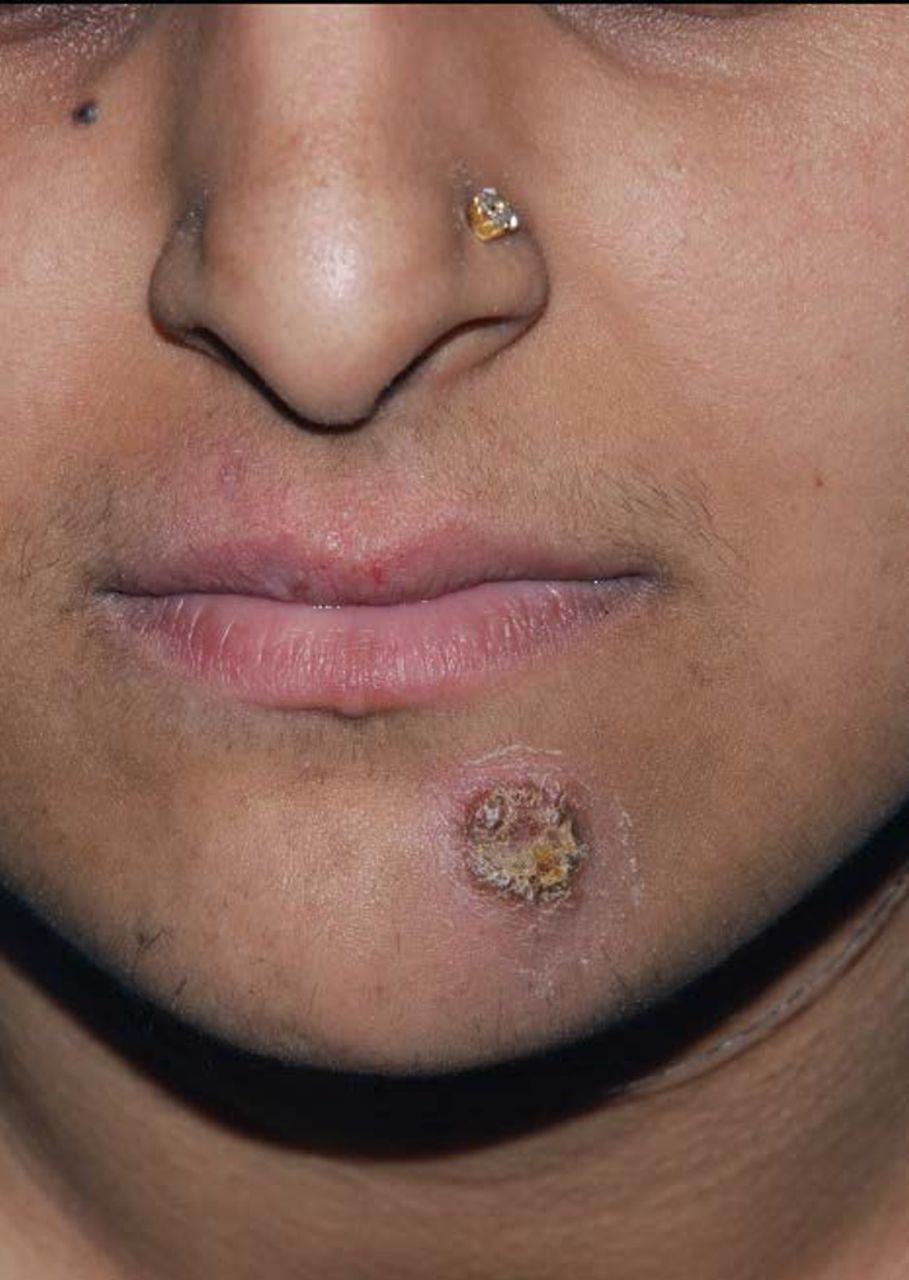
(BMJ) – The 5-yo son of a farmer presented with a 1-wk history of swelling of his left eyebrow. Scrapings from the eyebrow confirmed the diagnosis. What is it?

|
Psoriasis
|
|
Scabies
|
|
Atopic dermatitis
|
|
Mycosis fungoides
|
|
Kerion
|
