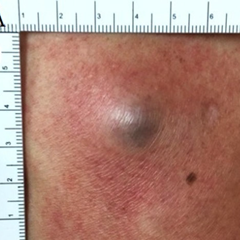
(BMJ)—A 51-yo man had a painful nodule on his R medial calf x4 days. He’d had varicose veins bilaterally on the lower limbs for >4y. No trauma hx or other sx. Exam: tender, red-purple ~2x2-cm nodule with surrounding rash. U/S confirmed the dx. What is it?
|
Superficial venous thrombosis
|
|
Abscess with cellulitis
|
|
Angiokeratoma
|
|
Deep vein thrombosis
|
|
Hematoma
|
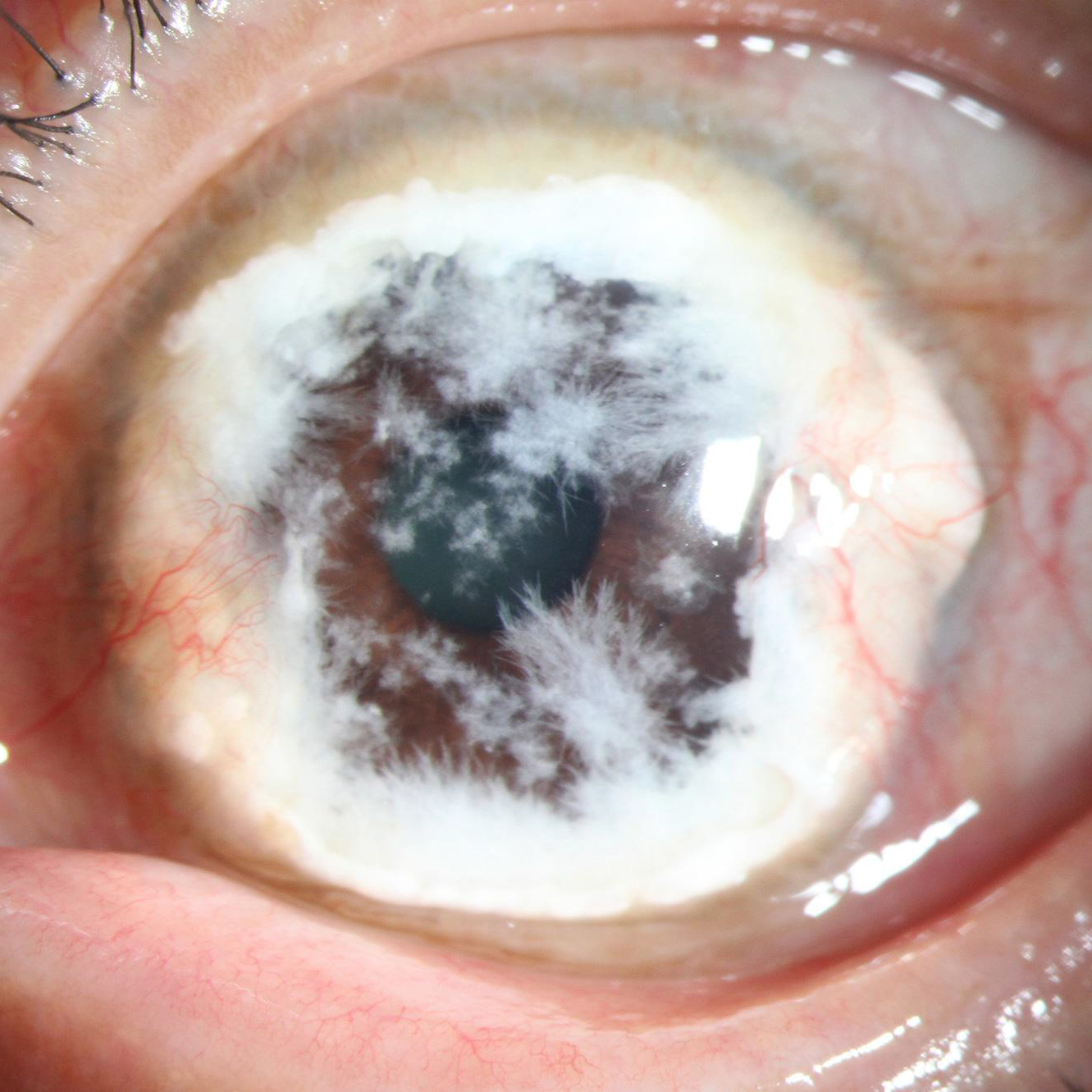
(BMJ)—A man in his 60s had blurred vision and bilateral eye redness x3y. Slit-lamp exam: bilateral peripheral dense corneal deposits with snowflake-like needle-shaped crystals extending centrally. Labs: calcium WNL, elevated uric acid. What’s the cause?
|
Streptococcus viridans infection
|
|
Multiple myeloma
|
|
Uric acid crystal deposition
|
|
Schnyder crystalline corneal dystrophy
|
|
Cystinosis
|
(epocrates)—A 63-yo female w/ HTN, hyperlipidemia, CHF, afib, and peripheral vascular dz initially presented w/ general malaise, an episode of weakness at home, knee pain, and stinging skin pain in her arms and legs, w/ AST 351 units/L and ALT 131 units/L. Atorvastatin was discontinued, and 4 days later, the pt presented w/ dark urine, generalized weakness, increased muscle and skin pain throughout her body, and creatine kinase (CK) 58,349 units/L (>50x the upper limit of normal). She was diagnosed w/ rhabdomyolysis and hospitalized for tx.
Meds: atorvastatin, carvedilol, digoxin, furosemide, spironolactone, rivaroxaban, and sacubitril/valsartan.
Which drug combo most likely caused the rhabdomyolysis?
Meds: atorvastatin, carvedilol, digoxin, furosemide, spironolactone, rivaroxaban, and sacubitril/valsartan.
Which drug combo most likely caused the rhabdomyolysis?

|
digoxin and atorvastatin
|
|
furosemide and atorvastatin
|
|
carvedilol and sacubitril/valsartan
|
|
atorvastatin and sacubitril/valsartan
|
(PubMed)—A 57-yo man w/ HIV and COPD presented w/ recurrent rib fractures, centripetal adiposity, and abdominal and inguinal striae. Dx: Cushing syndrome. Meds include ritonavir-containing HAART regimen, aspirin, clopidogrel, fluticasone/salmeterol, niacin, omeprazole, and pravastatin.
Which drug combo could have caused Cushing syndrome?
Which drug combo could have caused Cushing syndrome?

|
fluticasone and clopidogrel
|
|
clopidogrel and ritonavir
|
|
fluticasone and ritonavir
|
(Epilepsy Behav Case Rep)—A 44-yo man w/ hx of Marfan syndrome, mechanical mitral valve replacement, and tx-resistant epilepsy presented for an INR check 4wk after starting a new medication for intractable seizures. His INR had increased from 2.2 (before the new agent was added) to 6.7, leading the primary care physician to adjust the warfarin dosage to maintain an INR w/in a therapeutic range of 2 to 3.
Current meds: warfarin, cannabidiol, lamotrigine, levetiracetam.
Which drug was most likely to have resulted in the increased INR?
Current meds: warfarin, cannabidiol, lamotrigine, levetiracetam.
Which drug was most likely to have resulted in the increased INR?

|
lamotrigine
|
|
cannabidiol
|
|
levetiracetam
|
(Ment Health Clin)—A 58-year-old White female with a BMI of 33.6 kg/m2 and hx of recurrent major depression, generalized anxiety disorder, restless leg movements, onychomycosis, and alcohol use disorder presented with intensification of severe depression, intolerable anxiety, and restlessness. A commercial pharmacogenetic testing platform classified the patient as a normal metabolizer for CYP3A4 and CYP2D6. Her serum trough aripiprazole level was 207.5 ng/mL, which is 18% higher than the guideline-based dose-related reference concentration.
Meds: albuterol inhaler prn, aripiprazole, aspirin, cholecalciferol, ferrous sulfate, fluticasone/umeclidinium/vilanterol, lisinopril, lorazepam prn, metoprolol, pantoprazole, and terbinafine.
Which drug combo could have caused the elevated aripiprazole levels and akathisia?
Meds: albuterol inhaler prn, aripiprazole, aspirin, cholecalciferol, ferrous sulfate, fluticasone/umeclidinium/vilanterol, lisinopril, lorazepam prn, metoprolol, pantoprazole, and terbinafine.
Which drug combo could have caused the elevated aripiprazole levels and akathisia?

|
aripiprazole and pantoprazole
|
|
aripiprazole and lorazepam
|
|
aripiprazole and terbinafine
|
|
aripiprazole and lisinopril
|
